Dietary Avoidance for Food Allergy Frequently Asked Questions (FAQ)
This document has been developed by ASCIA, the peak professional body of clinical immunology/allergy specialists in Australia and New Zealand. ASCIA information is based on published literature and expert review, is not influenced by commercial organisations and is not intended to replace medical advice. For patient or carer support contact Allergy & Anaphylaxis Australia or Allergy New Zealand.
This information is for people with food allergy, and should be used with the ASCIA dietary guides for common allergy causing foods, available on the ASCIA website:
allergy.org.au/patients/food-allergy/ascia-dietary-avoidance-for-food-allergy
![]() ASCIA PCC Dietary Avoidance Food Allergy FAQ 2023280.23 KB
ASCIA PCC Dietary Avoidance Food Allergy FAQ 2023280.23 KB
Q 1: What do people with food allergy need to manage their condition?
It is important to note that anyone with food allergy should have:
- Regular review by their doctor and a clinical immunology/allergy specialist as required.
- Advice from a dietitian if there are multiple food allergies to make sure nutritional needs are met.
- Dietary Guides to provide information about foods that need to be avoided, and information about alternative foods that can provide important nutrients. Dietary avoidance should only be undertaken when a food allergy is suspected whilst waiting for medical confirmation, or when a food allergy has been medically confirmed.
- An adrenaline (epinephrine) injector if they are considered to be at risk of a severe allergic reaction (anaphylaxis).
- An ASCIA Action Plan for Anaphylaxis (red) if an adrenaline injector has been prescribed.
- An ASCIA Action Plan for Allergic Reactions (green) if an adrenaline injector has not been prescribed.
Q 2: Why is it important to read and understand food labels?
Many manufactured foods contain common allergy causing foods (food allergens), but it is not always easy to find the allergen information on the product packaging.
Ingredients or processes can be changed by manufacturers at any time without notice, so it is important to always check food labels when buying and preparing food every time you purchase the product, even if it has been a ‘safe’ food in the past,
For short, easy to understand videos about how to read and understand food labels for food allergy, scan this QR code or visit the National Allergy Council food allergy education website www.foodallergyeducation.org.au

Q 3: What information on food labels is required by law?
The Food Standards Code identifies common food allergens that must be declared on a food label if the allergen is contained in the food as:
- An ingredient.
- Part of a compound ingredient.
- A food additive.
- A processing aid.
In February 2021, there was a change in the Food Standards Code about the way food allergen information is provided on product labels. The standards in the Australia New Zealand Food Standards Code are legislative instruments under the Legislation Act 2003, which means they are laws which require food suppliers to comply.
This change requires allergen information to be declared in a specific format and location on food labels, and using simple, plain English terms in bold font, known as Plain English Allergen Labelling (PEAL).
There is a transition timeline for food companies to implement these changes, so it may not be until 2026 when all product labels will reflect this change. Therefore it will be important to know how to read labels that comply with the old and new laws.
Under the old law, allergens that must be declared are peanuts, tree nuts, cow’s milk (dairy), egg, soy, fish, shellfish (crustaceans), sesame, gluten and lupin. The source of the gluten (such as wheat) must also be declared.
Q 4: What are the new Plain English Allergen Labelling (PEAL) regulations?
The new PEAL regulations require:
- The same consistent names being used for the common food allergens.
- A ‘summary statement’ beginning with the word ‘contains’, that lists the allergens in the food.
- The summary statement to be located next to the ingredient list, which can be above, below or on either side of the ingredient list.
- Common food allergens to be declared as shown in the following table:
| Food |
Required name for declarations - ingredient list |
Required name for other declarations - summary statement
|
|
egg |
egg |
egg |
|
fish |
fish |
fish |
|
lupin |
lupin |
lupin |
|
milk |
milk |
milk |
|
mollusc |
mollusc |
mollusc |
|
crustacea |
crustacean |
crustacean |
|
peanut |
peanut |
peanut |
|
sesame seed |
sesame |
sesame |
|
soybean |
Soy, soya or soybean |
soy |
| Tree nuts | ||
|
almond |
almond |
almond |
|
Brazil nut |
Brazil nut |
Brazil nut |
|
cashew |
cashew |
cashew |
|
hazelnut |
hazelnut |
hazelnut |
|
macadamia |
macadamia |
macadamia |
|
pecan |
pecan |
pecan |
|
pine nut |
pine nut |
pine nut |
|
pistachio |
pistachio |
pistachio |
|
walnut |
walnut |
walnut |
| Gluten containing cereals | ||
|
wheat |
wheat |
wheat; |
|
barley |
barley |
gluten |
|
oats |
oats |
gluten |
|
rye |
rye |
gluten |
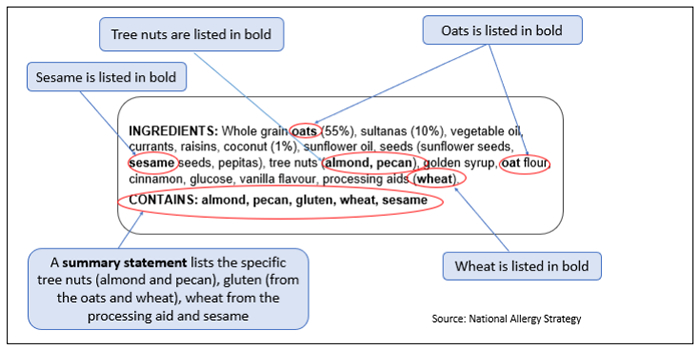
Examples of how food allergens must be declared on a food label under the new law is shown above.
For more information about the Food Standards Code, visit the Food Standards Australia New Zealand (FSANZ) website www.foodstandards.gov.au
Q 5: What are precautionary allergen statements?
Voluntary information on food labels includes precautionary allergen statements, which are used to declare cross contamination risk (such as ‘may contain...’), and these are not compulsory for food manufacturers.
It is important that people with food allergy discuss what to do about foods that include precautionary allergen statements with their clinical immunology/allergy specialist.
Q 6: What does ‘Free from’ products mean?
Some products are manufactured specifically to replace or exclude an allergen, such as ‘gluten free’. Even if the product is labelled ‘free from’, it is important to check the ingredients list for food allergens, as well as checking for precautionary allergen statements, such as ‘may contain’.
If choosing a ‘free from’ product, check that the preparation instructions do not require the addition of a food that is a confirmed food allergen for you or your child.
Q 7: What mistakes can be made when purchasing foods?
Examples of mistakes that can occur when purchasing foods include:
- Food labels are not read or understood.
- A person does not clearly disclose their allergy when purchasing unpackaged foods from a food outlet such as a bakery, café or restaurant.
- Waitstaff not communicating important information about a customer’s allergy to the chef.
- Chef does not check the ingredients in a product prepared offsite.
- Food services assuming that a small amount of the food allergen is safe.
- A family member forgets to check ingredients or disclose food allergens.
Q 8: Why does eating out require advanced planning?
It is important to plan ahead and communicate about food allergy:
- When eating out
- Travelling
- With institutions before starting school, children’s education and care, universities and workplaces.
- With hospitals before being admitted.
Providing information about your food allergy in advance increases the likelihood that they will be able to provide appropriate food which allows you to manage your food allergy.
When eating out, it is important to be assertive and clear. Before ordering, advise food service staff about your allergy clearly, and ask questions about ingredients, food preparation, storage and service.
If you are not sure that the food is suitable, do not eat it. If you have been prescribed an adrenaline injector, do not eat unless you have it with you.
Q 9: How can safe meals be prepared and served at home?
When preparing and serving food at home it is important to:
- Choose appropriate ingredients.
- Teach other household members and visitors about not sharing food and drinks.
- Be aware of cross contamination when storing, preparing and serving foods:
- Use separate cooking equipment.
- Prepare allergen free food first.
- Ensure adequate cleaning.
Q 10: How does cross contamination occur?
Cross contamination occurs when food allergens come into contact with a food that does not contain that allergen. This is similar to cross contamination that can occur with bacteria between raw and cooked meats.
Possible sources of cross contamination during include:
- During processing:
- Shared manufacturing lines for different products containing different ingredients.
- Shared packaging lines for different products containing different ingredients.
- Transport and storage of ingredients, particularly where spills can occur.
- At the point of purchase:
- Food sold in bulk containers and served using shared utensils.
- Delicatessen items due to use of the same serving utensils or cross contamination from a meat and cheese slicer.
- Food preparation using shared equipment:
- Knives, blenders, cutting boards, frying pans and deep fryers and barbecues.
- A different toaster should be used for people with wheat allergy.
- Food service:
- Buffets are especially high risk for many reasons, including food from one container being spilled into another food container and the same utensils being used for multiple food items. Even when separate utensils are provided, other customers may contaminate food by using the wrong utensil.
- Juice bars are high risk as the equipment may not be cleaned properly in between preparing different juices.
Q 11: What additional precautions can be taken for children with food allergies?
- For very young and mobile children with food allergy, consider not having the allergen in the home.
- If you decide to keep the food allergen in the home, you may consider reducing risk of exposure by:
- Having a shelf or container in the pantry and fridge for suitable foods for the child with food allergy.
- For very young children with food allergy, consider storing the food allergen/s out of reach or in a locked cupboard.
- Make sure that everyone who looks after your child (relatives, babysitters, friends, children’s education and care services, and school staff), fully understands your child’s food allergies, and how important it is that your child avoids the food they are allergic to. They should also know how to treat an allergic reaction, in case the child accidentally eats the food.
- Children should be encouraged from a young age to ask a trusted adult whether they are allowed to eat foods they may be given.
- If the child has been prescribed an adrenaline injector, make sure it is easily accessible at all times, and teach everyone who looks after your child to know when and how to use the device.
- Make sure the child sees their usual doctor for an updated ASCIA Action Plan, renewal of their adrenaline injector prescription and re-training in its use. The ASCIA Action Plan includes a recommended date for when the child next needs to see their doctor.
Q 12: When can baked egg and milk be eaten?
- Some children who are allergic to milk or egg may be able to eat baked egg or milk if this advice is given by their clinical immunology/allergy specialist.
- Children with milk or egg allergy should only be given baked milk or egg when supervised by a parent.
- Parents should not expect children’s education and care (CEC) staff to give foods containing baked milk or baked egg to their child with a milk or egg allergy when they are at a CEC service.
Q 13: Other than eating the food, are there other ways to contact with food allergens?
- Touching or smelling may trigger mild allergic symptoms but it is unlikely to cause anaphylaxis, as the food allergen usually needs to be eaten.
- Some cosmetics, shampoos, lotions, medications and alternative therapy products contain food allergens, and it is not mandatory to include allergen information on these product labels.
- People with food allergies should wash their hands after handling pet food, as this can contain allergens.
- For information about food allergens in medicines, visit the Therapeutic Goods Administration (TGA) website https://www.tga.gov.au/community-qa/allergies-and-medicines
© ASCIA 2023
Content updated December 2023
For more information go to www.allergy.org.au/patients/food-allergy and
www.allergy.org.au/patients/food-other-adverse-reactions
To support allergy and immunology research go to www.allergyimmunology.org.au/donate
